Clinical Case
Some case studies to illustrate the range of orthopaedic surgeries performed at our centre.
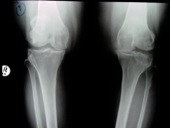
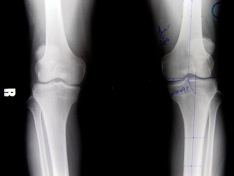
Rheumatoid Arthritis and Valgus Deformity Knee
Pre-Op
54 year old female with rheumatoid arthritis and valgus deformity left knee.

Post-Op
Patient had restoration of limb alignment and relief of knee pain.


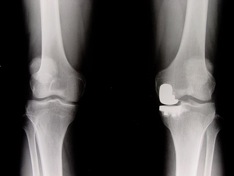
Pre-Op
Malunion femur with Knee osteoarthritis in a 54 year old female Chinese.
Stages
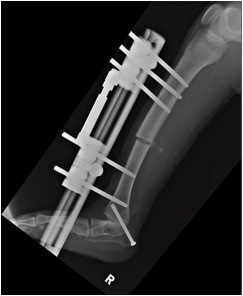
Open comminuted fracture femur treated with debridement and external fixator.


Later, treated with acute shortening and stabilization wit Ilizarove fixator for chronic osteomyelitis.


Healed but developed malunion and knee osteoarthritis, treated with intra-articular correction and knee replacement.


Post-Op 2nd surgery
Good restoration alignment and pain relief.


Patient had knee replacement done later for opposite knee also with good result.

Happy patient with good pain relief and knee motion.



Club Feet Treated with Ponseti Method
Pre-Op
3 months old baby with bilateral club feet.

Post-Op
Tendo Achilles release done with Ponseti bar / shoes.

Progress
8 months old. Excellent correction of both clubfeet.

8 Plate for Knock Knee Deformity in Child
Pre-Op
Preop unilateral right knock knee deformity.


Post-Op
8-plate inserted to distal femur via a small 2 cm incision to correct knock knee deformity.


Progress
1 year post surgery with 8-plate

18 months post surgery showing complete correction

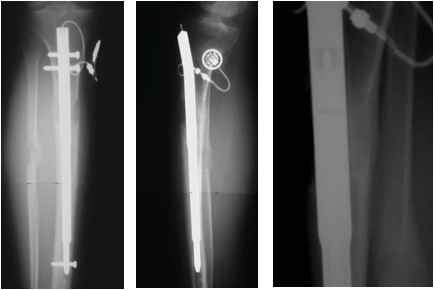
Retrograde ISKD for 3 cm Femur Shortening
Pre-Op
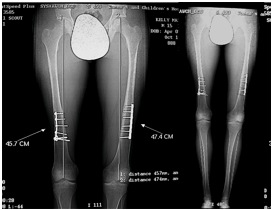
3 cm shortening femur secondary to coxa vara in a 16 year old female.


Post-Op
2 months post surgery. Retrograde ISKD nail inserted showing 3 cm lengthening.


4 months post surgery with good callus formation.

1 year post surgery. Leg length equalised.
Before

1 year post surgery

Progress
Excellent return of hip and knee motion after one year.



Perthes Disease in 9 Year Old Boy
Pre-Op
9 year old boy with Salter type B Perthes disease hip and lateral subluxation.
Intra-Op
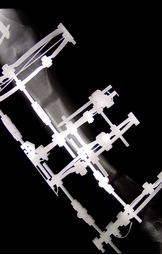
Distraction arthrodiastasis using Orthofix monolateral fixator.

Follow-Up
4 months on fixator.


Progress
Good hip remodeling and symptomatic improvement of hip.


Post Ilizarov Deformity
Pre-Op
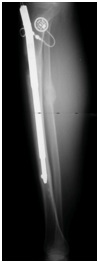
Hypertrophic non-union tibia with deformity in 54 year old female.

Post-Op
Ilizarov compression with fibular osteotomy.

Progress
Healing nonunion and deformity corrected.


Total Elbow Replacement
Pre-Op
56 years old Malaysian lady with rheumatoid arthritis with previous bilateral knee replacements done. Now, has pain and chronic swelling right elbow.
Before knee replacement
After total knee replacement

Elbow showing rheumatoid changes.

Post-Op
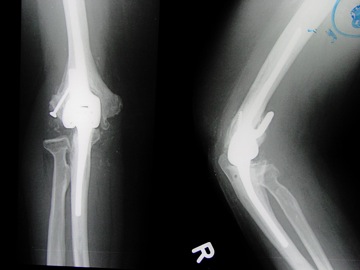
Progress
Good relief of elbow pain and excellent function.


Bilateral Knee Replacement
Pre-Op
62 years old lady with severe varus both knees and osteoarthritis.

Post-Op
Underwent bilateral knee replacements.

Follow-Up

Uni Comparmental Knee Replacement
Pre-Op
52 years old Malay male with chronic left knee pain due to uni compartmental arthritis.

Post-Op
Had uni compartmental knee replacement in view of relatively young age and mono compartmental arthritis.

Progress
Good relief of knee pain and full return of knee motion.


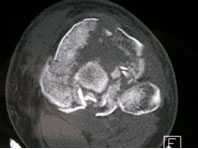
Tibial Plateau Fracture
Pre-Op
39 years old male Malaysian motorcyclist collided with a car.
Closed Schatzker VI Fracture Left Tibial Plateau
X-Rays


CT Scan


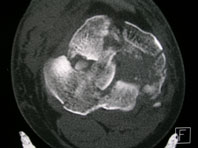
Surgery Stages
Lateral tibial plateau elevated and wire inserted.

2nd wire inserted into elevated lateral tibial plateau.

Bone Tunnel Drilled.

Punch inserted through tunnel and bone graft inserted.

Cross wires inserted.

Cannulated Screws.

Ring Fixator inserted.

Anterior Cortex Angulation.

Corrected with interfragmentary screw.

Post-Op
Alignment maintained with restoration of joint height.


Post-Op
After frame removal and union.



Good return of knee motion soon after frame removal.


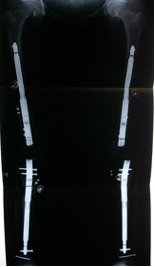
Bilateral Severe Leg Deformities
Pre-Op
12 year old Indonesian female Chinese girl with severe bilateral leg bowing due to congenital renal hypophosphatemia.
Walks with O-shaped deformity over both legs since young and short stature.


Stages
Underwent staged osteotomies for femur and tibia at separate intervals.
Femur done using acute correction with osteotomies at 2 levels and intramedullary nailing.
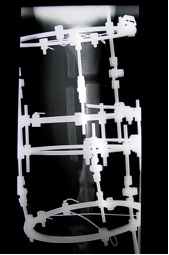
Six months later bilateral tibia double-level osteotomy and Ilizarov fixator applications.
Post-Op
Acute correction femoral deformities with nailing.

Tibia gradual correction at 2 levels with Ilizarov frame.
Final Result

Before


After



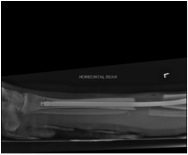
Tibia Lengthening with Fitbone
Pre-Op
- Male
- Amyoplasia
- Type 1 Diabetes
- Post bilateral release of the knees and osteotomies 1991
- Post R ETA and calcaneal osteotomy 3/94
- Limb Length Discrepancy of 3.5cm R, 1.7 cm Femur and 1.8 cm Tibia
- Back pain

Post-Op
Immediate.


20 Days Post Surgery.


- 19 mm distraction
- No pain
- Regained preoperative range in motion (ROM) in knee and ankle
30 Days Post Surgery.


- Lengthening of 29 mm – pelvis equal
- Patient feels comfortable
- Full ROM (same as pre-operatively)
- Note proximal migration of distal fibula
- Ceased lengthening
- Now Consolidation Phase with partial weight bearing (PWB)
Progress
4 months post surgery.

- No pain, asymptomatic
- Consolidation of 3 cortices - anterior no callus formation
- Full weight bearing (FWB) now
- No restrictions
6 Months Postoperative. Callus formation anteriorly.
24 Months Postoperative.

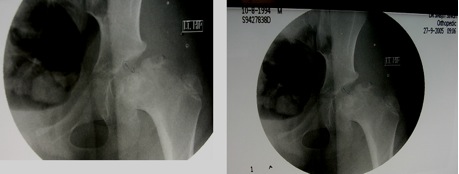
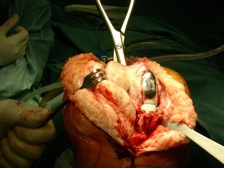
Hip Surface Replacement
Pre-Op
44 year old female presenting with severe left hip pain and limping X-rays showed early osteoarthritis of the hip joint.


Intra-Op
Guide wire in centre femoral neck.


ASR head and cup.


Post-Op

Cosmetic Leg Lengthening with Fitbone
Pre-Op
31 years old female with constitutional short stature of height 152 cm. Wanted height gain of 8 cm.

Post-Op
2 Fitbone nails in femur and 2 Fitbone nails inserted in tibia at one surgery.

3cm length in both femur and 5cm length gain in both tibia obtained with callus formation.
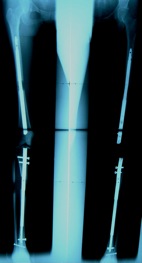
Progress
After nails removed two years later with excellent result and happy patient.

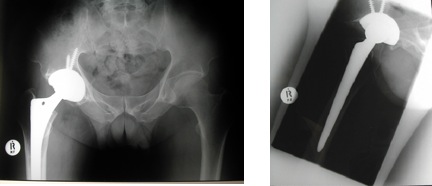
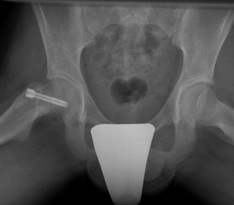
Total Hip Replacement Case #1
Pre-Op
33 years old female with hip pain due to avascular necrosis hips from chronic steroid ingestion.
Post-Op
Total hip replacement through minimally invasive single incision.


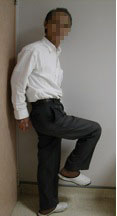
Progress
Happy patient with good pain relief and hip motion.


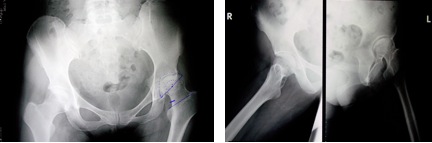
Total Hip Replacement Case #2
Pre-Op
65 years old male with pain and limping right hip due to osteoarthritis.

Post-Op
Total hip replacement done via minimally invasive single incision.
Progress
Grateful patient with pain relief and good hip motion.

Valgus Knee Deformity
Pre-Op
Standing AP of valgus deformity left knee in a 15 year old Indonesian girl

Post-Op
Closing wedge corrective osteotomy done and held with a DCS plate


Final AP standing showing good correction and union in 3 months

Comparison
Before Surgery

After Surgery

DDH - 4 Years Old Child
Pre-Op
4 year old child with right Development Dysplasia of the Hip (DDH)

Positive galleazi sign due to difference in leg length

Intra-Op
Hip spica applied immediately after surgery

Post-Op
Open reduction, femoral and pelvic osteotomy done successfully

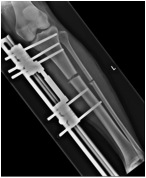
Valgus Right Leg with 3 cm Shortening from Polio
Pre-Op
Valgus right leg with 3 cm shortening in 41 year old Indian female


Progress
Acute correction and lengthening using supracondylar femoral osteotomy with “Lengthening Over Nail”

Post-Op

Follow Up
After fixator removal, static locking



Valgus and length corrected


Slipped Femoral Epiphsysis in a Child
Pre-Op
- 13 year-old Chinese boy
- Complained of right groin pain and limp for 5 months worse past 2 weeks
- Slightly overweight (55kg)
- Antalgic gait
- Right lower limb externally rotated at hip
- Movements of right hip restricted in all planes

AP X-Ray

Frog-Lateral X-ray

Post-Op
In-situ internal fixation with cannulated cancellous screw


Follow-Up
- 9 Months Post-Op
- Asymptomatic
- On examination:
- No limb length discrepancy
- Full and painless range of motion (right hip)
X rays-slip (9 months arrested and healed)

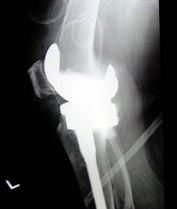
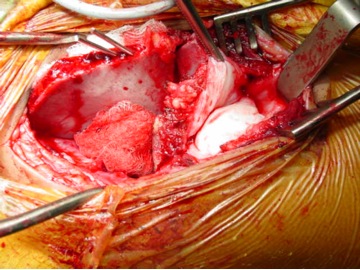
Elderly female with failed Unilateral Knee Replacement
Pre-Op
Elderly female with failed Unilateral Knee Replacement


Progress
Revised to Total Knee Replacement - note extensive bone loss after removal


Revision TKR with wedges and stems to compensate for extensive bone loss



Post-Op
X-rays showing TKR implant with good alignment


25 year old lady with constitutional short stature interested in “height-gain surgery”
Post-op Xrays - 2 weeks
Right Leg


Left Leg

4 months - 7cm distraction
Right Leg


Left Leg


Exchange nailing at 4 months with locked static AO tibia nails
Right Leg


Left Leg

13 years old Sri Lankan child
Pre-Op X-Rays


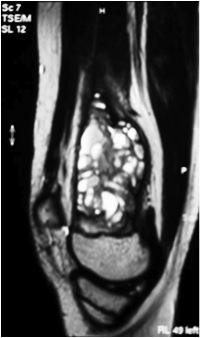
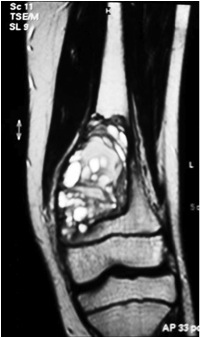
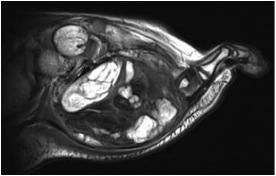
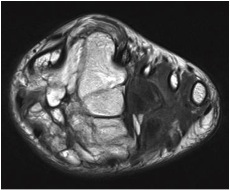
Pre-Op MRI
Intra-Op curettage and bone grafting with tutoplast bone chips


Immediate Post-Op X-rays with clearance of tumor and bone graft chips in-situ


Post-Op X-Rays: Good healing of tumor site at 3 months post surgery


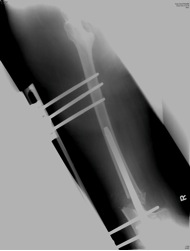
16 year old boy with 5 cm shortening right leg and procurvatum / valgus deformity tibia. Previous Ilizarov lengthening done at age 3 years
Pre-Op



Post-Op: Monolateral fixator with ankle cacaneotibial screw to prevent equinus

1 month post distraction


3 months post distraction


Conversion to internal solid tibia nail-shortening / deformity corrected


Final correction with good bone healing and limb equalised, mild residual ankle equinus




3 years old boy with progressive large swelling over foot
Pre-Op


Pre-Op MRI
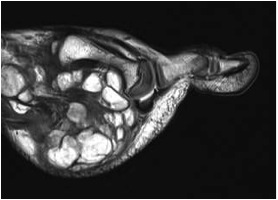
Intra-Op


Post-Op




 Adult Orthopaedic
Adult Orthopaedic